Dialysis
- Home
- Specialities
- Dialysis
Best Dialysis Centre in India For Kidney Disease Treatment

Dialysis is a treatment for people whose kidneys are failing. When you have kidney failure, your kidneys don’t filter blood the way they should. As a result, wastes and toxins build up in your bloodstream. Dialysis does the work of your kidneys, removing waste products and excess fluid from the blood.
Why Choose Aykai?
Aykai’s dialysis hospital in Ludhiana redefines patient care by combining advanced medical expertise with modern facilities. Each dialysis session is performed in a safe, comfortable setting, ensuring patients receive the highest level of care. Our dedicated team focuses on delivering personalized treatment plans tailored to each individual’s unique health needs and lifestyle. Committed to excellence, we provide comprehensive support, from cutting-edge technology to compassionate care, ensuring optimal outcomes and improved quality of life. Recognized as a leading dialysis center, Aykai stands out for its holistic approach, addressing every aspect of kidney care with unmatched precision and dedication.
Who needs dialysis?
People who have kidney failure, or end-stage renal disease (ESRD), may need dialysis. Injuries and conditions like high blood pressure, diabetes and lupus can damage kidneys, leading to kidney disease.
Some people develop kidney problems for no known reason. Kidney failure can be a long-term condition, or it can come on suddenly (acute) after a severe illness or injury. This type of kidney failure may go away as you recover.
There are five stages of kidney disease. In stage 5 kidney disease, healthcare providers consider you to be in end-stage renal disease (ESRD) or kidney failure. At this point, kidneys are carrying out around 10% to 15% of their normal function. You may need dialysis or a kidney transplant to stay alive. Some people undergo dialysis while waiting for a transplant.
Haemodialysis
What is hemodialysis?
With hemodialysis, a machine removes blood from your body, filters it through a dialyzer (artificial kidney) and returns the cleaned blood to your body. This 3- to 5-hour process may take place in a hospital or a dialysis center three times a week.
You can also do hemodialysis at home. You may need at-home treatments four to seven times per week for fewer hours each session. You may choose to do home hemodialysis at night while you sleep.
What happens before hemodialysis?
Before you start hemodialysis, you’ll undergo a minor surgical procedure to make it easier to access the bloodstream. You may have:
- Arteriovenous fistula (AV fistula): A surgeon connects an artery and vein in your arm.
- Arteriovenous graft (AV graft): If the artery and vein are too short to connect, your surgeon will use a graft (soft, hollow tube) to connect the artery and vein.
AV fistulas and grafts enlarge the connected artery and vein, which makes dialysis access easier. They also help blood flow in and out of your body faster.
If dialysis needs to happen quickly, your provider may place a catheter (thin tube) into a vein in your neck, chest or leg for temporary access.
Your provider will teach you how to prevent infections in your fistula or graft. This provider will also show you how to do hemodialysis at home if you choose to do so.
Peritoneal Dialysis
With peritoneal dialysis, tiny blood vessels inside the abdominal lining (peritoneum) filter blood through the aid of a dialysis solution. This solution is a type of cleansing liquid that contains water, salt and other additives.
Peritoneal dialysis takes place at home. There are two ways to do this treatment:
- Automated peritoneal dialysis uses a machine called a cycler.
- Continuous ambulatory peritoneal dialysis (CAPD) takes place manually.
Vascular Access
Vascular access is essential for hemodialysis, allowing blood removal, filtration, and return through a surgically created vein. Long-term options include AV fistulas and grafts, while venous catheters are for short-term use.
What is an Arteriovenous Fistula?
An AV fistula is a connection between an artery and a vein, created by a transplant surgeon, usually in the arm. It increases blood flow and pressure in the vein, making it larger and stronger for reliable access during hemodialysis. This access is essential as untreated veins collapse under repeated needle use. AV fistulas offer better blood flow, last longer, and have lower infection and clot risks than other access types. Before surgery, Doppler ultrasound mapping evaluates blood vessels. The procedure, performed under local anesthesia, often requires outpatient care. Maturation takes 2–3 months.

What is an Arteriovenous Graft?
An AV graft is a looped plastic tube connecting an artery to a vein, providing access for hemodialysis. It’s usable within 2–3 weeks but is more prone to infection and clotting than an AV fistula. Proper care can extend its lifespan to several years.

Set Up Vascular Access Early
Vascular access should be created well before starting hemodialysis to allow AV fistulas or grafts time to mature. Early preparation prevents complications like narrow veins or clots. Providers can teach exercises to enlarge veins and preserve arm vessels for successful access creation.
What is a Venous Catheter?
A venous catheter is a short-term hemodialysis access tube inserted into a vein in the neck, chest, or groin. It has two lines to connect to the dialysis machine. Typically used when immediate dialysis is needed, it’s placed by a nephrologist or interventional radiologist under local anesthesia. Catheters can last weeks or months but are prone to infections, clots, and vein scarring. For extended use, a tunneled catheter, placed under the skin, reduces discomfort and complications but still carries risks. Venous catheters are temporary solutions until an AV fistula or graft matures or if long-term surgical options are unsuccessful.

What Problems Could a Vascular Access Cause?
Vascular access—AV fistula, AV graft, or venous catheter—can lead to complications requiring treatment or surgery. Common issues include infections and low blood flow caused by clotting. Properly formed AV fistulas are less likely to develop these problems compared to grafts or catheters, though no access type is risk-free.
AV grafts are prone to narrowing or clotting, potentially requiring angioplasty or surgical repair. Venous catheters, intended for short-term use, have the highest risk of infection and clotting. Treatments include antibiotics for infections and blood thinners like warfarin for clots. If unsuccessful, the catheter may need replacement.
How to Protect Vascular Access
Patients should keep the access clean, avoid pressure or injury, and monitor daily for signs of infection or issues. Only use the access for dialysis and avoid restrictive clothing, heavy lifting, or blood pressure checks on the access arm.
Sustained Low-Efficiency Dialysis (SLED)
SLED is a renal replacement therapy designed for critically ill patients with acute kidney failure. Combining the benefits of conventional dialysis and continuous therapies, it operates for prolonged durations (6-12 hours) at a slower rate, minimizing hemodynamic instability.
Sustained low-efficiency dialysis (SLED) is a renal replacement therapy (RRT) treatment for critically ill patients with acute renal failure (ARF). SLED is a hybrid of conventional intermittent hemodialysis (IHD) and continuous renal replacement therapy (CRRT). It involves:
- 8 hours of hemodialysis (HD) six days a week
- Blood flow of 200 ml/min
- Dialysate flows of 350 ml/min
- Hemofiltration with 1 L of saline/h
SLED has several advantages, including:
- Lower risk of hypotension: The prolonged session duration of SLED results in lower ultrafiltration rates, which minimizes the risk of intradialytic hypotension.
- Can be performed without anticoagulation: SLED can be performed without anticoagulation in many cases.
- Flexible treatment schedule: SLED allows patients to be freed from the dialysis apparatus for most of the day.
- Easy to perform: SLED is easy to perform.
Benefits:
- Suitable for unstable patients.
- Gradual fluid and toxin removal.
- Less strain on the heart and blood pressure.
Procedure: Blood is filtered through a dialysis machine using a specialized catheter. It utilizes slower blood and dialysate flow rates compared to standard dialysis, ensuring stability.
Treatment: SLED is performed in ICU settings under medical supervision, addressing kidney dysfunction while prioritizing patient stability.
Continuous Renal Replacement Therapy (CRRT)
CRRT is a dialysis technique used for critically ill patients with acute kidney failure, especially those with unstable blood pressure. It continuously removes waste, toxins, and excess fluid over 24 hours, mimicking natural kidney function.
Benefits:
- Gentle fluid and toxin removal.
- Stabilizes blood pressure.
- Reduces risk of complications for critically ill patients.
Procedure: Blood is circulated through a machine using a catheter, where waste is filtered and replaced with clean fluids. The slow, continuous process ensures better tolerance for unstable patients.
Treatment: CRRT is performed in ICU settings, providing constant kidney support under close monitoring.
Clinical Team
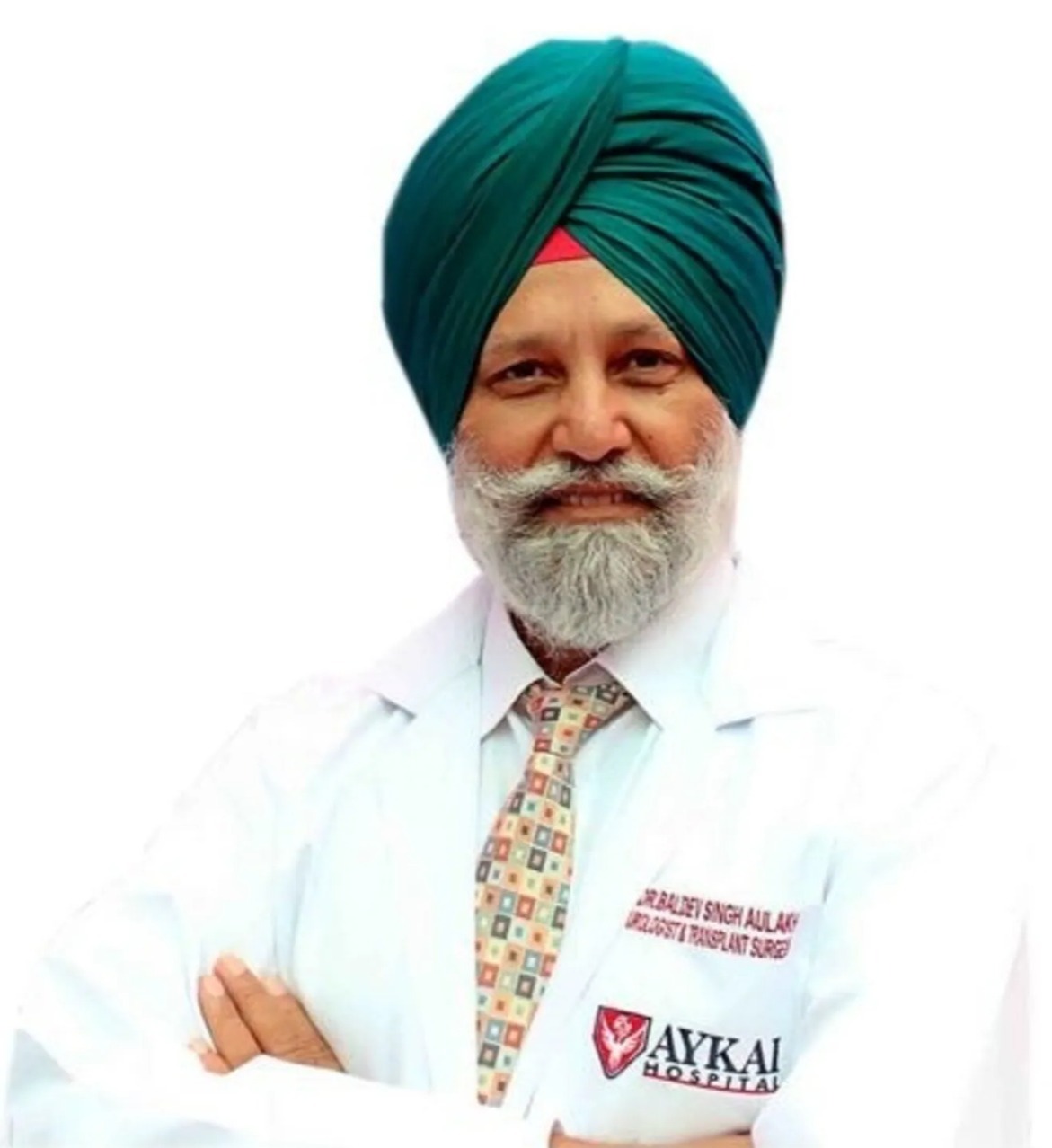
Dr. Baldeev Singh Aulakh
Urologist, Laparoscopic, Robotic and Transplant Surgeon

Dr. Amit Tuli
(Urologist and Andrologist)

Dr. Vivekanand Jha
(Nephrologist)

Dr. Naresh
(Urologist)

Dr. Gaurav
(Urologist)

Dr. Himanshu
(Urologist)

Dr. Pranav Arora
(Anesthesia)
Are you having health problems? Contact us today!
Call Us 24/7: 0161-525 25 25

